In the ongoing debate over masks and mask mandates, the common messages at both extremes lack substance. Empty slogans aren’t helping anybody. The civic bloodstream could use an injection of specifics, and a healthy dose of nuance could save lives.
As of this month’s revised guidance, the Centers for Disease Control recommends mask use in indoor public spaces for both vaccinated and unvaccinated people in COVID-19 hotspots such as Shelby County, and virtually everywhere else across the country.
It’s well past time we quantify the benefit masks provide.
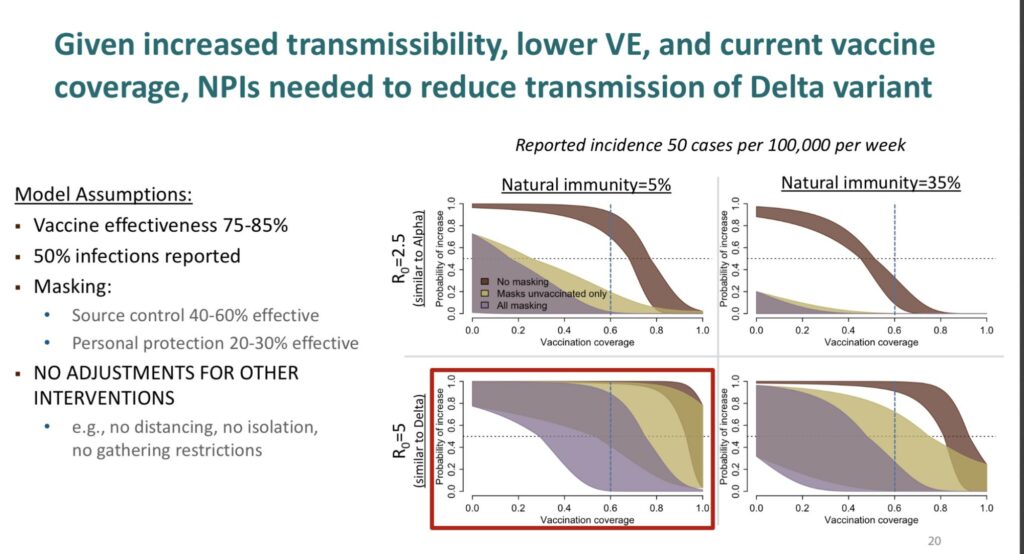
In an internal slide accompanying its reversal on mask use for vaccinated people, the CDC assumes masks are 40-60% effective as source control and 20-30% effective as personal protection.
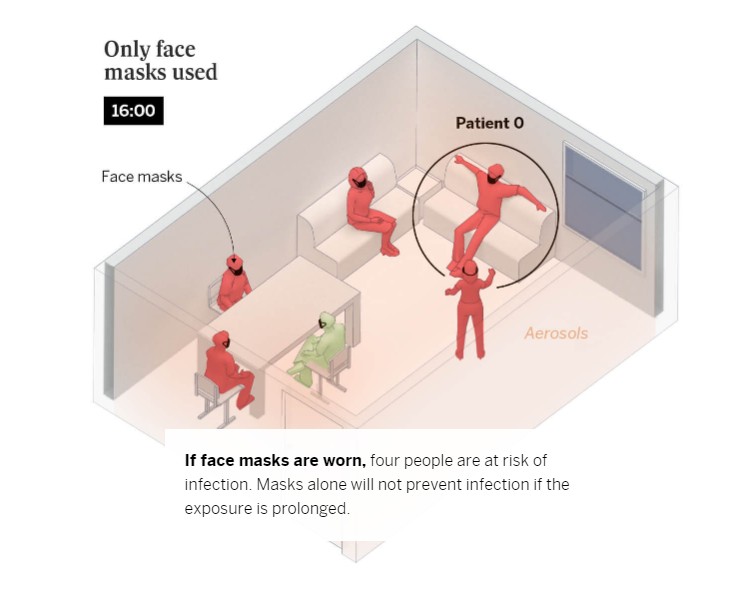
Let’s explore what that model could mean in practice. Say you are in a room with an infected person, and you’re both wearing masks. Half of the virus particles the other person breathes out could be captured by their mask, and about a fifth of the escapee microdroplets could be filtered by your mask. Thanks to masks, huzzah, you might breathe in only about 40% of the infected particles.
Unfortunately, that’s still enough for you to become infected.
Real world examples bear this out. The CDC’s report on mask mandates through the end of 2020 shows a 1.8 percent reduction in case growth rates and a 1.9 percent reduction in death growth rates after 81-100 days, the longest post-implementation period studied.
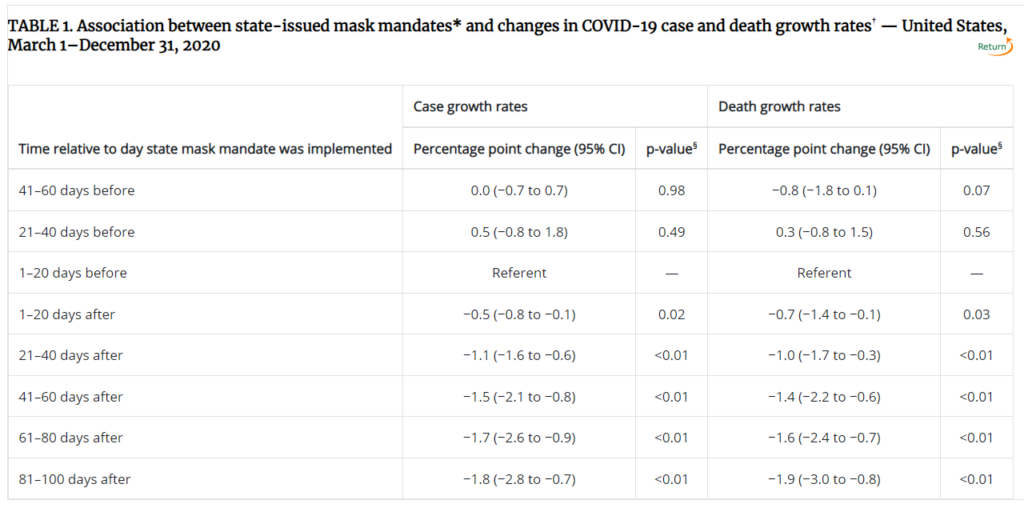
That’s not nothing. With an aggregate benefit this slight, however, it’s no wonder we have an ongoing disagreement about whether masks “work.”
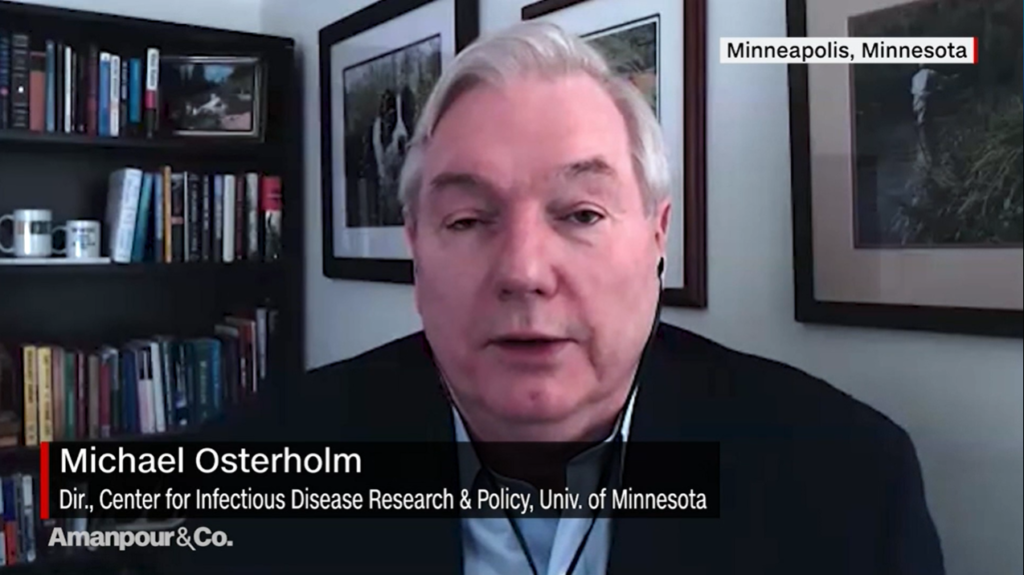
Epidemiologist Dr. Michael Osterholm was a member of the Biden COVID-19 Advisory Board and is the Director of the Center for Infectious Disease Research and Policy at the University of Minnesota. He says public health has “done a disservice to the public” on masks, telling PBS that cloth masks “only have very limited impact in reducing the amount of virus that you inhale in or exhale out” and extending only about five minutes of protection to someone in a room with the virus present.
Masks can either “work,” or not, depending on how you define the term. If what you mean to say is masks can provide people with a modest level of protection, especially when combined with other preventative measures, I have no objection. May the odds be ever in your favor.
If by “masks work” you mean wearing a piece of fabric over your face will absolutely prevent you from catching COVID-19, I’m sorry, but that’s simply wrong. Thousands and thousands of people have been infected despite their diligent use of masks.

An over-emphasis on masking and too much confidence in masks can be detrimental for at least a few reasons, made more troublesome by healthcare “experts” who insist on dumbing down the message.
First, refusing to admit the obvious limits to the benefit of masking leads many to believe masks are the equivalent of vaccines, if not better.
The discussion of vaccines often includes efficacy percentages and talk of breakthrough cases and possible side-effects. But no such defects, percentages or specifics are brought into the discussion of masks. This leads many to believe they will be fine going into the world with just a mask on and that they don’t need to take the trouble to get vaccinated. That conclusion leaves people at greater risk.
Second, the intensity concerning masks is so strong that it causes us to lose sight of the more important goal of reaching herd immunity, preferably through vaccination. Requiring fully vaccinated people to remain masked eliminates what has been an incentive to get the stick – to be rid of masks.
Is our primary goal keeping people masked indefinitely or giving them a better shot at avoiding severe complications and death? If it’s the latter, let’s put the bulk of our efforts toward building confidence in vaccines, and let individuals consider their own risk profile, free of mandates.
Finally, the simplistic emphasis on masks erodes the public’s trust in health officials and “experts.”
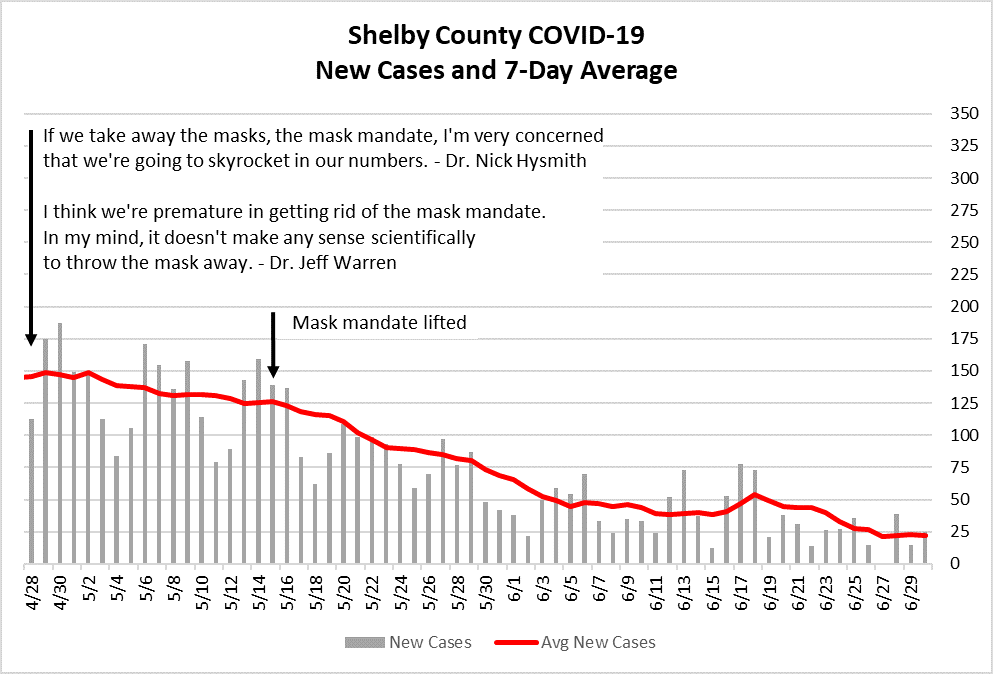
When we hear physicians make failed pronouncements about cases skyrocketing if a mask mandate is lifted (that didn’t happen) or suggesting no students will be placed in quarantine if all classrooms are required to wear masks (good luck), we can easily conclude the experts have no idea what they are talking about.
We all witnessed what happened last year. We lived through it. We followed the health directives, and the spread continued anyway. We know the guidance offers no guarantees.
“I’ve been really disappointed with my colleagues in public health for not being more clear about what can masking do or not do.”
Dr. Michael Osterholm, Dir., Center for Infectious Disease Research and Policy, University of Minnesota
To restore trust, the public health community needs to act as a partner in the fight against COVID-19, not as a benevolent dictator. Public health should offer recommendations backed by sound science and provide individuals with access to reliable and specific information about what might truly help them.
The mask wars have no victor. COVID-19 is the enemy, not our masked or unmasked neighbors.

